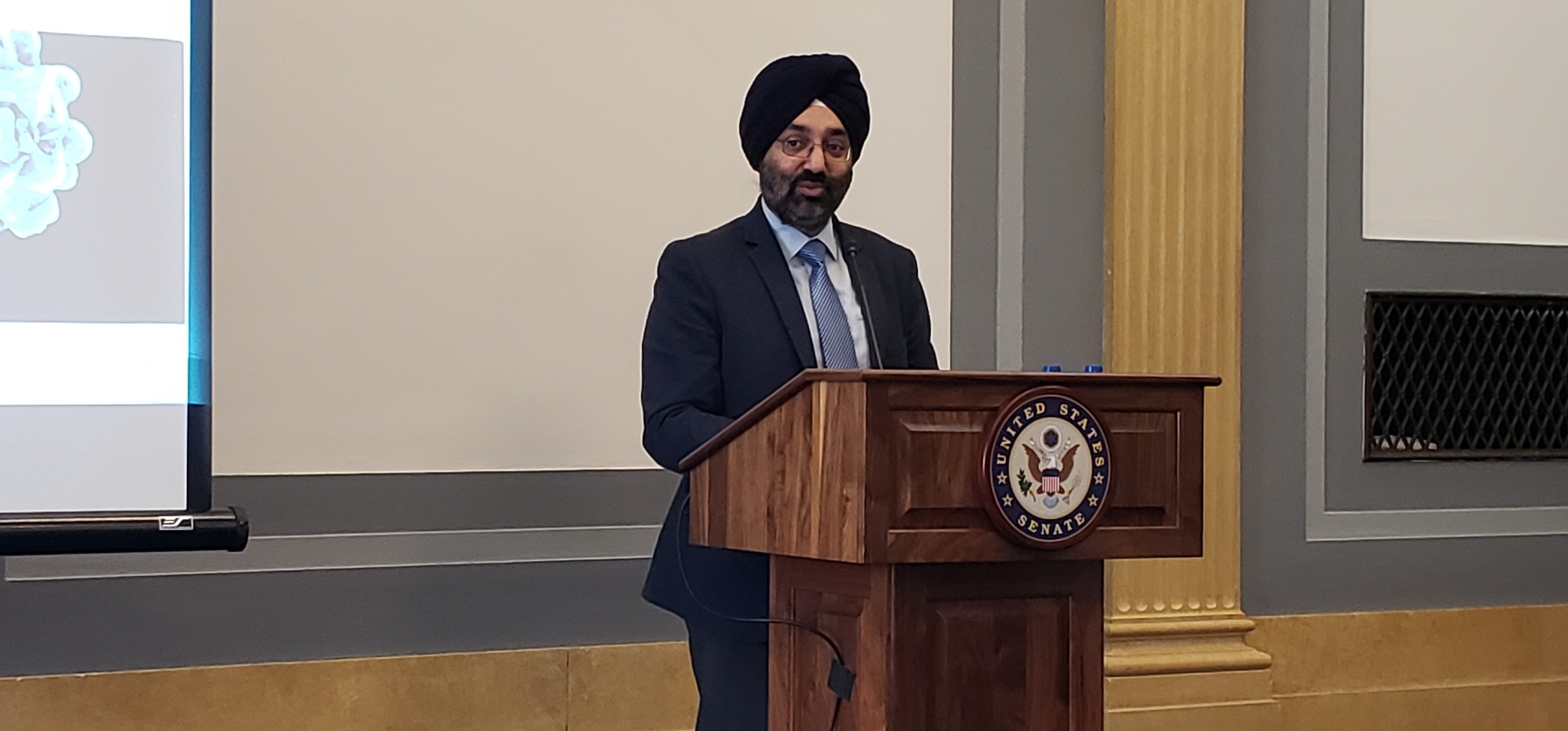
On Nov. 13, ASBMT President-Elect Navneet Majhail, MD, MS, and Joseph Alvarnas, MD, participated in a Congressional Roundtable on Medicare’s reimbursement systems for CAR-T cell therapies. They provided a detailed overview of CAR-T cell therapy and examined potential solutions to keep Medicare’s reimbursement systems current and at pace with research and best practices.
ASBMT sat down with Majhail to discuss how the meeting went, and what solutions ASBMT leadership would like to see when it comes to reimbursement methodology.
ASBMT: It’s quite an honor to be asked to participate in a Congressional Roundtable – why do you think ASBMT was asked to participate?
Majhail: CAR-T cell therapies are highly innovative and have changed the treatment paradigm for our patients. However, they are exorbitantly priced – to the extent that their cost may end up causing barriers to access for patients. As CAR-T’s were emerging in the commercial space, ASBMT recognized the need to advocate for adequate coverage and has taken a major leadership role in this area. ASBMT’s executive committee and board have consciously dedicated significant resources and effort to ensure we keep working on policy and coverage challenges in this area. The Congressional Roundtable was an opportunity for ASBMT, ASH, Lymphoma Research Foundation and NCCN – organizations that represent patients, providers and centers – to come together and educate our policy makers about issues around Medicare coverage. Given our strong advocacy work in this area, it was a natural fit for ASBMT to be an influential voice in this conversation. I do want to acknowledge Stephanie Farnia, who till recently was our Director for Health Policy and Strategic relations, since she was instrumental in helping ASBMT get to this place.
What are some of the primary concerns, from your perspective, about the current state of Medicare’s reimbursement systems?
Medicare coverage for the two commercial products in the market (Yescarta® and Kymriah™) is woefully inadequate. We were really appreciative that CMS provided some relief in its FY 2019 national Inpatient Prospective Payment System (IPPS) rule by expanding the scope of and payment associated with the MS-DRG that covers CAR-T and for providing guidance on the use of a New Technology Add-on Payment (NTAP) that will help reimburse a proportion of the drug costs. However, to put things into perspective, the reimbursement provided by MS-DRG 016 will be ~39,000 and a center will be able to obtain a maximum of $186,500 for drug costs under the NTAP mechanism. Collectively, this will still amount to >50% shortfall in the cost of providing CAR-T therapy to patients with Medicare coverage, which in the long-term is not sustainable and will create significant access barriers to patients.
What’s the next step in this conversation with Congressional leaders?
To summarize some of the high-level points the ASBMT has been emphasizing to Congressional leaders and CMS: first, we recognize and acknowledge that the current CAR-T therapies are very expensive and that from a CMS perspective these prices are not sustainable, especially given the tsunami of cell therapies that is coming. We also recognize and acknowledge the costs incurred by industry around research and development and commercialization of these drugs. However, at the end of the day it cannot be business as usual and we need newer payment models to address coverage for CAR-T’s and similar expensive therapies. It will take CMS some time to figure this out, and the ASBMT has suggested some innovative payment models to consider. Coming up with creative ways to pay for these therapies is not easy, is definitely required, and will need careful deliberation and time. Meanwhile, there are some shorter term “fixes”. CMS can implement a detailed, transparent, and robust coding/billing structure to obtain high quality data that will help it better understand the actual cost of delivering care and come up with mechanisms to reimburse the drug costs closer to their true acquisition costs (e.g., implement a cost-to-charge ratio of 1.0 for the CAR-T product). Also CMS should not incentivize administration of this therapy in the outpatient setting since most patients do need to be hospitalized for management of toxicities with the current commercial CAR-T therapies. The letter submitted jointly by ASBMT and ASH elaborates on these proposed immediate and long-term solutions.
Anything else you would like to add?
As clinicians, we just want to take care of our patients. There is nothing more devastating than to tell a patient that he or she cannot receive a potentially life-saving therapy because they have no or inadequate coverage. At this time, the financial risk for providing this therapy is squarely on the shoulders of providers, institutions, patients and payers. We need to move towards rational and responsible alternative payment models if the price of these therapies continues to be very high, and some of the newer models would involve the drug manufacturers to take on some risk. It will take some time to reach that state, and in the meantime ASBMT remains committed to carrying on advocacy at the local and national level so that our patients can receive the care they need.